27 History of Schizophrenia
History of schizophrenia

The term “schizophrenia” was coined by Eugen Bleuler.
The history of schizophrenia is complex and does not lend itself easily to a linear narrative. Accounts of a schizophrenia-like syndrome are rare in records before the 19th century. The earliest cases detailed were reported in 1797, and 1809. Dementia praecox, meaning premature dementia ( brain dementia of the young) was used by German psychiatrist Heinrich Schüle in 1886, and then in 1891 by Arnold Pick in a case report of hebephrenia (Disorganized schizophrenia, or hebephrenia, is a subtype of schizophrenia) In 1893 Emil Kraepelin used the term in making a distinction, known as the Kraepelinian dichotomy, between the two psychoses – dementia praecox, and manic depression (now called bipolar disorder). Kraepelin believed that dementia praecox was probably caused by a systemic disease that affected many organs and nerves, affecting the brain after puberty in a final decisive cascade. It was thought to be an early form of dementia, a degenerative disease. When it became evident that the disorder was not degenerative it was renamed schizophrenia by Eugen Bleuler in 1908.
The word schizophrenia translates roughly as “splitting of the mind” and is Modern Latin from the Greek roots schizein (σχίζειν, “to split”) and phrēn, (φρεν, “mind”) Its use was intended to describe the separation of function between personality, thinking, memory, and perception. Bleuler described four primary symptoms of schizophrenia. According to him, the ‘4A’s’ of schizophrenia were – ambivalence, autism, reduced association (or disassociation) of ideas and flat affect. In addition to this, Bleuler also observed that this disorder was different from dementia praecox, as some individuals recovered partially instead of progressively worsening.
The term schizophrenia used to be associated with split personality by the general population but that usage went into decline when split personality became known as a separate disorder, first as multiple identity disorder, and later as dissociative identity disorder. In 2002 in Japan the name was changed to integration disorder, and in 2012 in South Korea, the name was changed to attunement disorder to reduce the stigma, both with good results.
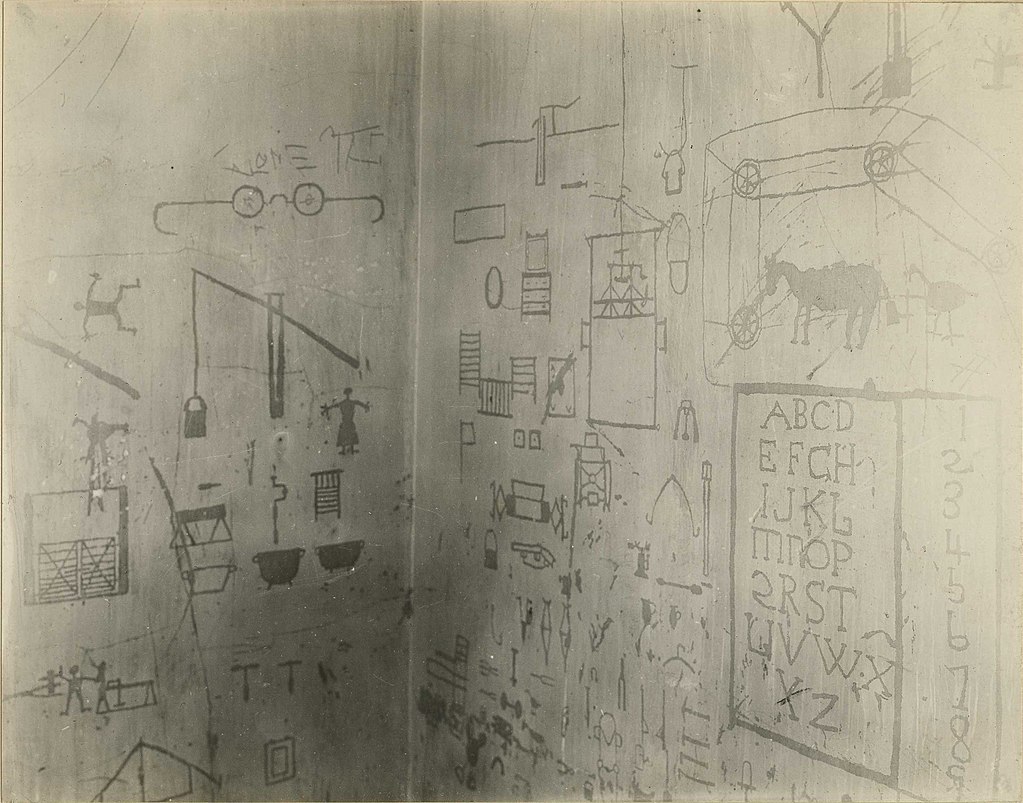 Scratch-drawings on the wall in St. Elizabeths Hospital made by a prisoner with “a disturbed case of dementia praecox”.
Scratch-drawings on the wall in St. Elizabeths Hospital made by a prisoner with “a disturbed case of dementia praecox”.
In the early 20th century, the psychiatrist Kurt Schneider listed the psychotic symptoms of schizophrenia into two groups of hallucinations, and delusions. The hallucinations were listed as specific to auditory, and the delusional included thought disorders. These were seen as the symptoms of first-rank importance and were termed first-rank symptoms (FRS). Whilst these were also sometimes seen to be relevant to the psychosis in manic-depression, they were highly suggestive of schizophrenia and typically referred to as first-rank symptoms of schizophrenia. Schneider formulated this list of first-rank symptoms in order to classify and separate schizophrenia from other psychotic disorders. The major first-rank symptoms include – hallucinations (auditory and somatic), thought insertion, thought broadcasting and delusional perception. The most common first-rank symptom was found to belong to thought disorders. Schneider’s first-rank symptoms have been instrumental in designing the diagnostic criteria for schizophrenia, however, the exact nature of these symptoms is not very thorough and they have been questioned. In 2013 the first-rank symptoms were excluded from the DSM-5 criteria. First-rank symptoms are seen to be of limited use in detecting schizophrenia but may be of help in differential diagnosis.
A molecule of chlorpromazine (brand name Thorazine), the first antipsychotic developed in the 1950s.
The earliest attempts to treat schizophrenia were psychosurgical, involving either the removal of brain tissue from different regions or the severing of pathways. These were notably frontal lobotomies and cingulotomies which were carried out from the 1930s. In the 1930s a number of shock therapies were introduced which induced seizures (convulsions) or comas. Insulin shock therapy involved the injecting of large doses of insulin in order to induce comas, which in turn produced hypoglycemia and convulsions. The use of electricity to induce seizures was developed, and in use as electroconvulsive therapy (ECT) by 1938. Stereotactic surgeries were developed in the 1940s. Treatment was revolutionized in the mid-1950s with the development and introduction of the first typical antipsychotic, chlorpromazine. In the 1970s the first atypical antipsychotic clozapine, was introduced followed by the introduction of others.
In the early 1970s in the US, the diagnostic model used for schizophrenia was broad and clinically-based using DSM II. It had been noted that schizophrenia was diagnosed far more in the US than in Europe which had been using the ICD-9 criteria. The US model was criticized for failing to demarcate clearly those people with a mental illness, and those without. In 1980 DSM III was published and showed a shift in focus from the clinically-based biopsychosocial model to a reason-based medical model. DSM IV showed an increased focus to an evidence-based medical model. DSM-5 was published in 2013 and introduced changes to DSM IV.
After an evolving through six editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM), the exact definition of schizophrenia still remains elusive. Initially, diagnosing schizophrenia was focused on the Kraepelinian concepts of the disorders poor outcome, chronicity and patients’ avolition. A broader definition of the disorder was reflected in DSM – I and DSM – II. These two editions used Bleuler’s symptoms as a reference and focused mainly on the interpersonal pathology and negative symptoms. The DSM – III and subsequently the DSM – III R and DSM – IV, adopted Kurt Schneider’s first-rank symptoms and highlighted them in addition to the chronic nature and lack of functioning seen in the disorder. The primary construct of the DSM – IV was seen to be reliable, had a fair amount of validity, but more importantly, was clinically relevant. Therefore the primary definition of schizophrenia remains unchanged in the DSM – 5.
Prior to the elimination of its subtypes, schizophrenia had the following distinct clinical subtypes – paranoid, undifferentiated, disorganized and catatonic, with the paranoid subtype being the most commonly diagnosed among patients. However, studies have shown that these subtypes are not reliable, are not stable over a period of time and have little or no prognostic value. In addition, these subtypes do not tend to occur together in families and many a time, patients present with more than one subtype. Finally, the subtypes mentioned above do not respond to any particular pattern of treatment and they cannot be inherited from parent to offspring. As a result, these subtypes of schizophrenia have now been eliminated. The DSM – 5 focuses on the psychopathological aspects of the disorder in order to more effectively address its heterogeneity which can have a higher validity, better use clinically and encourage measurement-based treatment. Along with these new approaches and with the help of the DSM – 5 in combining the neurobiological and genetic aspects of schizophrenia, it might be possible to unravel the true nature behind this mysterious disorder.
“History of Schizophrenia” is adapted from Abnormal Psychology by Coursehero, used under CC BY-SA: Attribution-ShareAlike.

