26 Phenomenology of Schizophrenia
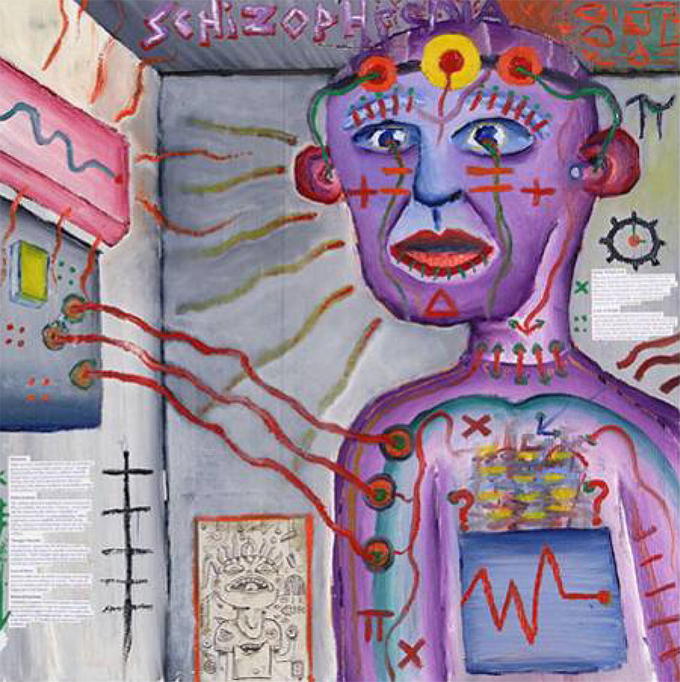 Schizophrenia: This self-portrait of a person with schizophrenia represents their perception of a distorted experience of reality.
Schizophrenia: This self-portrait of a person with schizophrenia represents their perception of a distorted experience of reality.
Most of you have probably had the experience of walking down the street in a city and seeing a person you thought was acting oddly. They may have been dressed in an unusual way, perhaps disheveled or wearing an unusual collection of clothes, makeup, or jewelry that did not seem to fit any particular group or subculture. They may have been talking to themselves or yelling at someone you could not see. If you tried to speak to them, they may have been difficult to follow or understand, or they may have acted paranoid or started telling a bizarre story about the people who were plotting against them. If so, chances are that you have encountered an individual with schizophrenia or another type of psychotic disorder. If you have watched the movie A Beautiful Mind or The Fisher King, you have also seen a portrayal of someone thought to have schizophrenia. Sadly, a few of the individuals who have committed some highly publicized mass murders may have had schizophrenia, though most people who commit such crimes do not have schizophrenia. It is also likely that you have met people with schizophrenia without ever knowing it, as they may suffer in silence or stay isolated to protect themselves from the horrors they see, hear, or believe are operating in the outside world. As these examples begin to illustrate, psychotic disorders involve many different types of symptoms, including delusions, hallucinations, disorganized speech and behavior, abnormal motor behavior, and negative symptoms such anhedonia/amotivation and blunted affect/reduced speech. Because the patient has lost contact with reality, we say that he or she is experiencing psychosis, which is a psychological condition characterized by a loss of contact with reality.
Even though schizophrenia is accompanied by a variety of symptoms, not all patients have all of them (Lindenmayer & Khan, 2006). As you can see in the Table below, “Positive, Negative, and Cognitive Symptoms of Schizophrenia,” the symptoms are divided into positive symptoms, negative symptoms, and cognitive symptoms (American Psychiatric Association, 2008; National Institute of Mental Health, 2010). Positive symptoms refer to the presence of abnormal behaviors or experiences (such as hallucinations) that are not observed in normal people, whereas negative symptoms (such as lack of affect and an inability to socialize with others) refer to the loss or deterioration of thoughts and behaviors that are typical of normal functioning. A third category of cognitive symptoms (the changes in cognitive processes that accompany schizophrenia) (Skrabalo, 2000) is also included in some descriptions of the disease. Both positive and negative symptoms are further characterized as motor, behavioral, and mood disturbances. Positive symptoms tend to be the easiest to recognize and they respond well to treatment. Negative symptoms appear to contribute more to poor quality of life, functional impairment, and to the burden on others than do positive symptoms. People with greater negative symptoms often have a history of poor adjustment before the onset of illness. Negative symptoms are less responsive to medication, and are the most difficult to treat. In some cases, negative symptoms can be misinterpreted as depression or laziness.
|
Positive, Negative, and Cognitive Symptoms of Schizophrenia. |
||
|
|
||
|
Positive symptoms |
Negative symptoms |
Cognitive symptoms |
|
Hallucinations |
Asociality and Social withdrawal |
Poor executive control |
|
Delusions |
Flat affect and anhedonia ( lack of pleasure in everyday life) |
Trouble focusing |
|
Disorganized thoughts and speech |
Avolition (a lack of motivation) and apathy |
Working memory problems |
|
Grossly disorganized behavior |
Alogia (a poverty of speech) |
Poor problem-solving abilities |
|
Inappropriate affect |
Lack of goal-oriented activity |
Slow processing speed |
|
Catatonic excitement |
Catatonic stupor |
|
|
|
Poor hygiene and grooming and Distorted sense of time |
|
Delusions are false beliefs that are often fixed, hard to change even when the person is presented with conflicting information, and are often culturally influenced in their content (e.g., delusions involving Jesus in Judeo-Christian cultures, delusions involving Allah in Muslim cultures). They can be terrifying for the person, who may remain convinced that they are true even when loved ones and friends present them with clear information that they cannot be true. There are many different types or themes to delusions:
Delusions of grandeur– belief they have exceptional abilities, wealth, or fame; belief they are God or other religious saviors
Delusions of control– belief that their thoughts/feelings/actions are controlled by others
Delusions of thought broadcasting– belief that one’s thoughts are transparent and everyone knows what they are thinking
Delusions of persecution– belief they are going to be harmed, harassed, plotted or discriminated against by either an individual or an institution
Delusions of reference– belief that specific gestures, comments, or even larger environmental cues are directed directly to them
Delusions of thought withdrawal– belief that one’s thoughts have been removed by another source

Under Surveillance: Abstract groups like the police or the government are commonly the focus of a schizophrenic’s persecutory delusions.
The most common delusions are persecutory and involve the belief that individuals or groups are trying to hurt, harm, or plot against the person in some way. These can be people that the person knows (people at work, the neighbors, family members), or more abstract groups (the FBI, the CIA, aliens, etc.). Other types of delusions include grandiose delusions, where the person believes that they have some special power or ability (e.g., I am the new Buddha, I am a rock star); referential delusions, where the person believes that events or objects in the environment have special meaning for them (e.g., that song on the radio is being played specifically for me); or other types of delusions where the person may believe that others are controlling their thoughts and actions, their thoughts are being broadcast aloud, or that others can read their mind (or they can read other people’s minds). It is believed that the presentation of the delusion is largely related to the social, emotional, educational, and cultural background of the individual (Arango & Carpenter, 2010). For example, an individual with schizophrenia who comes from a highly religious family is more likely to experience religious delusions (delusions of grandeur) than another type of delusion.
When you see a person on the street talking to themselves or shouting at other people, they are likely experiencing hallucinations. These are perceptual experiences that occur even when there is no stimulus in the outside world generating the experiences. They can be auditory, visual, olfactory (smell), gustatory (taste), or somatic (touch). The most common hallucinations in psychosis (at least in adults) are auditory, and can involve one or more voices talking about the person, commenting on the person’s behavior, or giving them orders. The content of the hallucinations is frequently negative (“you are a loser,” “that drawing is stupid,” “you should go kill yourself”) and can be the voice of someone the person knows or a complete stranger. Sometimes the voices sound as if they are coming from outside the person’s head. Other times the voices seem to be coming from inside the person’s head, but are not experienced the same as the person’s inner thoughts or inner speech.
Talking to someone with schizophrenia is sometimes difficult, as their speech may be difficult to follow, either because their answers do not clearly flow from your questions, or because one sentence does not logically follow from another. This is referred to as disorganized speech, and it can be present even when the person is writing. Speech that is not understandable is known as word salad ( confused or unintelligible mixture of seemingly random words and phrases). Among the most common cognitive impairments displayed in patients with schizophrenia are disorganized thought, communication, and speech. More specifically, thoughts and speech patterns may appear to be circumstantial or tangential. For example, patients may give unnecessary details in response to a question before they finally produce the desired response. While the question is eventually answered in circumstantiality, in tangentially, the patient never reaches the point. Another common cognitive symptom is speech retardation where the individual may take a long period of time before answering a question. Derailment, or the illogical connection in a chain of thoughts, is another common type of disorganized thinking. Although not always, derailment is often seen in illogicality, or the tendency to provide bizarre explanations for things.
These type of distorted thought patterns are often related to concrete thinking. That is, the individual is focused on one aspect of a concept or thing, and neglects all other aspects. This type of thinking makes treatment difficult as individuals lack insight into their illness and symptoms (APA, 2013).
Disorganized behavior can include odd dress, odd makeup (e.g., lipstick outlining a mouth for 1 inch), or unusual rituals (e.g., repetitive hand gestures). Abnormal motor behavior can include catatonia, which refers to a variety of behaviors that seem to reflect a reduction in responsiveness to the external environment. This can include holding unusual postures for long periods of time, failing to respond to verbal or motor prompts from another person, or excessive and seemingly purposeless motor activity.
Some of the most debilitating symptoms of schizophrenia are difficult for others to see. As we discussed earlier, these include what people refer to as negative symptoms or the absence of certain things we typically expect most people to have. For example, anhedonia or amotivation reflect a lack of apparent interest in or drive to engage in social or recreational activities. These symptoms can manifest as a great amount of time spent in physical immobility. Importantly, anhedonia and amotivation do not seem to reflect a lack of enjoyment in pleasurable activities or events (Cohen & Minor, 2010; Kring & Moran, 2008; Llerena, Strauss, & Cohen, 2012) but rather a reduced drive or ability to take the steps necessary to obtain the potentially positive outcomes (Barch & Dowd, 2010). Flat affect and reduced speech (alogia) reflect a lack of showing emotions through facial expressions, gestures, and speech intonation, as well as a reduced amount of speech and increased pause frequency and duration.
In many ways, the types of symptoms associated with psychosis are the most difficult for us to understand, as they may seem far outside the range of our normal experiences. Unlike depression or anxiety, many of us may not have had experiences that we think of as on the same continuum as psychosis. However, just like many of the other forms of psychopathology described in this book, the types of psychotic symptoms that characterize disorders like schizophrenia are on a continuum with “normal” mental experiences. For example, work by Jim van Os in the Netherlands has shown that a surprisingly large percentage of the general population (10%+) experience psychotic-like symptoms, though many fewer have multiple experiences and most will not continue to experience these symptoms in the long run (Verdoux & van Os, 2002). Similarly, work in a general population of adolescents and young adults in Kenya has also shown that a relatively high percentage of individuals experience one or more psychotic-like experiences (~19%) at some point in their lives (Mamah et al., 2012; Ndetei et al., 2012), though again most will not go on to develop a full-blown psychotic disorder.
Diagnostic Criteria
DSM-5 DIAGNOSTIC CRITERIA FOR SCHIZOPHRENIA
|
|
A. Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated): Delusions Hallucinations Disorganized speech (e.g., frequent derailment or incoherence) Grossly disorganized or catatonic behavior Negative symptoms (i.e., diminished emotional expression or avolition)
B. For a significant portion of the time since the onset of the disturbance, level of functioning in one or more major areas, such as work, interpersonal relations, or self-care, is markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, there is failure to achieve expected level of interpersonal, academic, or occupational functioning).
C. Continuous signs of the disturbance persist for at least 6 months. This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A (i.e., active-phase symptoms) and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or by two or more symptoms listed in Criterion A present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences).
D. Schizoaffective disorder and depressive or bipolar disorder with psychotic features have been ruled out because either 1) no major depressive or manic episodes have occurred concurrently with the active-phase symptoms, or 2) if mood episodes have occurred during active-phase symptoms, they have been present for a minority of the total duration of the active and residual periods of the illness.
E. The disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition.
F. If there is a history of autism spectrum disorder or a communication disorder of childhood onset, the additional diagnosis of schizophrenia is made only if prominent delusions or hallucinations, in addition to the other required symptoms of schizophrenia, are also present for at least 1 month (or less if successfully treated).
|
” |
As stated above, the hallmark symptoms of schizophrenia include the presentation of at least two of the following for at least one month: delusions, hallucinations, disorganized speech, disorganized/abnormal behavior, or negative symptoms. These symptoms create significant impairment in an individual’s ability to engage in normal daily functioning such as work, school, relationships with others, or self-care. It should be noted that presentation of schizophrenia varies greatly among individuals, as it is a heterogeneous clinical syndrome (APA, 2013).
While the presence of symptoms have to persist for a minimum of 6 months to meet criteria for a schizophrenia diagnosis, it is not uncommon to have prodromal symptoms that precede the active phase of the disorder and residual symptoms that follow it. These prodromal and residual symptoms are “subthreshold” forms of psychotic symptoms that do not cause significant impairment in functioning, with the exception of negative symptoms (Lieberman et al., 2001). Due to the severity of psychotic symptoms, mood disorder symptoms are also common among individuals with schizophrenia; however, these mood symptoms are distinct from a mood disorder diagnosis in that psychotic features will exist beyond the remission of depressive symptoms.
Prevalence of Schizophrenia. Schizophrenia affects around 0.3–0.7% of people at some point in their life. About 1.1% of adults have schizophrenia in the United States. Although schizophrenia can occur at any age, the average age of onset tends to be in the late teens to the early 20s for men, and the late 20s to early 30s for women. Onset in childhood, before the age of 12 can sometimes occur, however this is uncommon. A later onset can occur between the ages of 40 and 60, known as late onset, and also after 60 known as very late onset (also uncommon).
KEY TAKEAWAYS
Alogia
A reduction in the amount of speech and/or increased pausing before the initiation of speech.
Anhedonia/amotivation
A reduction in the drive or ability to take the steps or engage in actions necessary to obtain the potentially positive outcome.
Catatonia
Behaviors that seem to reflect a reduction in responsiveness to the external environment. This can include holding unusual postures for long periods of time, failing to respond to verbal or motor prompts from another person, or excessive and seemingly purposeless motor activity.
Delusions
False beliefs that are often fixed, hard to change even in the presence of conflicting information, and often culturally influenced in their content.
Disorganized behavior
Behavior or dress that is outside the norm for almost all subcultures. This would include odd dress, odd makeup (e.g., lipstick outlining a mouth for 1 inch), or unusual rituals (e.g., repetitive hand gestures).
Disorganized speech
Speech that is difficult to follow, either because answers do not clearly follow questions or because one sentence does not logically follow from another.
Flat affect
A reduction in the display of emotions through facial expressions, gestures, and speech intonation.
Hallucinations
Perceptual experiences that occur even when there is no stimulus in the outside world generating the experiences. They can be auditory, visual, olfactory (smell), gustatory (taste), or somatic (touch).
Negative symptom
Any behavior seen in people without the disorder that is lacking in the person with the disorder; a disorder of omission.
Positive symptom
Any behavior not seen in people without the disorder that correlates with a loss of contact with reality; a disorder of commission.
Psychopathology
Illnesses or disorders that involve psychological or psychiatric symptoms.
Psychosis
A severe mental disorder characterized by impairment in thoughts and emotion and often involving a loss of contact with external reality.
Volition
The mental power or ability of choosing; will.
“Phenomenology of Schizophrenia” is adapted from Abnormal Psychology by Coursehero, used under CC BY-SA: Attribution-ShareAlike.

